doi: 10.56294/cid202373
ORIGINAL
Evaluation of Burnout Syndrome and associated factors in primary care health personnel
Evaluación del Síndrome Burnout y factores asociados en personal sanitario de Atención Primaria
Lázaro Pablo Linares Cánovas1 ![]() *, Liyansis Bárbara Linares Cánovas2
*, Liyansis Bárbara Linares Cánovas2 ![]() , Yoelys Pereda Rodríguez1
, Yoelys Pereda Rodríguez1 ![]() , Beatriz Gallardo Hernández1, Martha María Pérez
Martín1, Adalina Linares Montano3
, Beatriz Gallardo Hernández1, Martha María Pérez
Martín1, Adalina Linares Montano3
1Policlínico Docente Universitarios Luis Augusto Turcios Lima. Pinar del Río, Cuba.
2Universidad de Ciencias Médicas de Pinar del Río. Pinar del Río, Cuba.
3Universidad de Sonora. Ciudad de Sonora, México.
Cite as: Cánovas LPL, Cánovas LBL, Rodríguez YP, Hernández BG, Martín MMP, Montano AL. Evaluation of Burnout Syndrome and associated factors in primary care health personnel. Community and Interculturality in Dialogue 2023;3:73. https://doi.org/10.56294/cid202373.
Submitted: 30-06-2023 Revised: 24-08-2023 Accepted: 31-10-2023 Published: 01-11-2023
Editor: Prof.
Dr. Javier González Argote ![]()
ABSTRACT
Objective: to evaluate Burnout syndrome and associated factors in health personnel of Primary Care.
Methods: observational, analytical, cross-sectional study, carried out in Pinar del Río during January 2023, in non-probabilistic sampling for convenience, of 127 participants, who met the inclusion criteria. The application of instruments such as the Maslach Burnout Inventory questionnaire, allowed obtaining the information that gave output to the studied variables, applying descriptive and inferential statistical methods. Medical ethics were respected.
Results: 66,9 % of the workers were women, with a median of 31 years of age. Resident physicians predominated (45,7 %), with a median of 8 years working in the sector. 73,2 % showed overload, with the emotional exhaustion dimension being the most affected. The presence of Burnout syndrome was associated with sleeping eight hours a day (p=0,016) and with satisfaction with economic income (p<0,001). The affectation of the emotional exhaustion dimension was statistically associated with sex, religion and sleeping eight hours a day (p<0,05). Depersonalization was associated with religion (p=0,001), sleeping eight hours a day (p=0,016), smoking (p=0,001) and satisfaction with economic income (p=0,011); while professional achievement was related to sleeping eight hours a day (p<0,001), adequate dietary habits (p=0,038) and satisfaction with economic income (p=0,016).
Conclusions: Burnout syndrome was evaluated in primary care health personnel, identifying the demographic characteristics, lifestyle and work variables of the sample, and their relationship with professional exhaustion.
Keywords: Burnout; Professional; Primary Health Care; Health Professionals; Occupational Health.
Resumen
Objetivo: evaluar el síndrome Burnout y los factores asociados, en personal sanitario de la Atención Primaria.
Métodos: estudio observacional, analítico, transversal, realizado en Pinar del Río durante enero de 2023, en muestreo no probabilístico por conveniencia, de 127 participantes, que cumplieron los criterios de inclusión. La aplicación de instrumentos como el cuestionario Maslach Burnout Inventory, permitieron obtener la información que dio salida a las variables estudiadas, aplicándose métodos de estadística descriptiva e inferencial. Se respetó la ética médica.
Resultados: el 66,9 % de los trabajadores eran mujeres, con una mediana 31 años. Predominaron los médicos residentes (45,7 %), teniéndose una mediana de 8 años trabajando en el sector. El 73,2 % mostró sobrecarga, siendo la dimensión cansancio emocional la más afectada. La presencia del síndrome de Burnout estuvo asociada con dormir ocho horas diarias (p=0,016) y con la satisfacción con los ingresos económicos (p<0,001). La afectación de la dimensión cansancio emocional estuvo asociada estadísticamente con el sexo, religión y dormir ocho horas diarias (p<0,05). La despersonalización estuvo asociada con la religión (p=0,001), dormir ocho horas diarias (p=0,016), el tabaquismo (p=0,001) y la satisfacción con los ingresos económicos (p=0,011); mientras la realización profesional se relacionó con dormir ocho horas diarias (p<0,001), hábitos dietéticos adecuados (p=0,038) y la satisfacción con los ingresos económicos (p=0,016).
Conclusiones: fue evaluado el síndrome Burnout en personal sanitario de la Atención Primaria, identificándose las características demográficas, el estilo de vida y las variables laborales de la muestra, y su relación con el agotamiento profesional.
Palabras clave: Agotamiento Profesional; Atención Primaria De Salud; Personal De Salud; Salud Laboral.
INTRODUCTION
Primary Care (PC), defined as essential healthcare accessible to the entire community, stands as the core of the healthcare system. Its practitioners bear the responsibility of overseeing the majority of occurrences that contribute to a deterioration in the health status of individuals, families, and communities. Within this framework, the depletion of its human resources may precipitate the onset of Burnout Syndrome (BS), a condition distinguished by physical, psychological, and emotional disturbances arising from inadequate management of chronic work-related stress; consequently, it is recognized as a public health concern.(1)
Herbert Freudenberger first delineated this syndrome in 1974, and although its definition was not included in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-V), or the International Classification of Diseases and Related Health Problems, tenth edition (ICD-10), owing to its not-recognition as a distinct disease; it had been mentioned in the International Classification of Diseases (ICD-10) under code Z73.0. As of January 1st, 2022, the ICD-11 came into effect, and as declared during the 72nd World Health Assembly of the WHO (May 2019), Burnout Syndrome is officially acknowledged as a work-related issue classified under QD85.(2,3,4)
Healthcare providers within PC are susceptible to the onset of Burnout Syndrome, a condition with notable consequences for their physical health. This is accompanied by job dissatisfaction and an intention to leave the profession, thereby contributing to the devaluation of the doctor-patient relationship and a diminution in the quality of care delivered. As a result, the service provider, the patient, and the healthcare system itself are all affected.(5,6,7)
Studies have suggested that up to 78 % of primary care physicians undergo feelings of burnout, while rates among residents and nurses fall within the range of 45,50 %.(8,9,10,11,12) Woodward et al.(13) assert that high rates of burnout are escalating at an alarming pace. In this context, although the literature provides a significant amount of information on this topic from North America, Europe, and Asia, there is a paucity of reports from developing countries, with Latin America being one of the regions lacking sufficient information. In these areas, both the quantity and methodological quality of the conducted reports are not sufficient to accurately identify the magnitude and prevalence of the phenomenon, as well as the factors associated with its development.(14,15) Therefore, the present study was conducted with the aim of addressing BS and its associated factors in primary care healthcare personnel.
METHODS
An observational, analytical, cross-sectional study was conducted among healthcare personnel operating in two primary care units in the municipality of Pinar del Río during January 2023. Through non-probabilistic sampling for convenience, a sample of 127 participants was selected, who met the inclusion criteria (being of legal age, working during the study period in the Luis Augusto Turcios Lima and Pedro Borrás Astorga polyclinics, and agreeing to participate in the study by signing the informed consent) and exclusion criteria (having worked in Primary Care for less than six months).
In this study, a strategy for information gathering was the participant's self-completion of an online questionnaire (Google Forms service) with encrypted access through a password. The responses were automatically recorded in an exportable database. The questionnaire was structured into two sections: the first encompassed an Ad hoc survey collecting sociodemographic and work-related information, while the second section included the Maslach Burnout Inventory instrument. This facilitated the data collection that led to the studied variables: age, sex, marital status, religion, skin color, having children, sleeping eight hours daily, tobacco use, practice of physical exercise, proper dietary habits, profession (within the occupation categories, family physicians [residents or specialists], nurses, social workers, pharmacists, psychologists, odontologists, physiotherapists, and nutritionists were included), satisfaction with economic income, professional experience, and the presence of BS.
The Maslach Burnout Inventory (MBI) questionnaire, adapted to Spanish, served as the measurement tool for assessing BS. This instrument for evaluating professional exhaustion consists of 22 items that assess the three dimensions constituting the construct:
• Emotional Exhaustion (EE): 9 items [1-2-3-6-8-13-14-16-20]
• Depersonalization (DP): 5 items [5-10-11-15-22]
• Personal Accomplishment (PA): 8 Items [4-7-9-12-17-18-19-21])
Each item was evaluated on a 7-point Likert scale ranging from 0 to 6 (0 = never, 1 = a few times a year or less, 2 = once a month or less, 3 = a few times a month, 4 = once a week, 5 = a few times a week, 6 = every day). For the evaluation of each dimension, the following cutoff points indicating impairment were applied: EE > 26, DP > 9, and PA < 34. Additionally, for the diagnosis of BS, the presence of two or three affected spheres was considered. This instrument has been validated for use in Cuba, where its construct validity and reliability are affirmed, demonstrating adequate internal consistency with a Cronbach's alpha coefficient of 0,77.(16,17)
For the statistical analysis of the acquired data, IBM SPSS version 26 statistical software was utilized. Univariate analysis of categorical variables involved the use of absolute frequencies and percentages, whereas medians and interquartile ranges were applied for quantitative variables (given the previous demonstration of the non-compliance with the normality assumption). Bivariate analysis encompassed Pearson's chi-square (X2) test, Mann-Whitney U test, Kruskal-Wallis H test, and Spearman's correlation. The predetermined level of statistical significance was set at p < 0,05.
For the execution of this research, international ethical guidelines for health-related research involving human subjects, as elaborated by the Council for International Organizations of Medical Sciences (CIOMS) in collaboration with the World Health Organization (WHO), along with adherence to the Helsinki declaration, were followed.(18) Furthermore, prior to commencing the study, approval was obtained from the Ethics and Research Committee of the institutions where the research was conducted. The questionnaire was subsequently distributed to all participants, accompanied by an explanation of the research's objectives, the voluntary nature of participation and completion, as well as the assurance of confidentiality and anonymity throughout the study.
RESULTS
The sample exhibited a median age of 31 years (IQR: 27-41), with a predominance of females (66,93 %), individuals with white skin color (79,53 %), atheists (48,82 %), and those without children (62,99 %). Approximately 33,86 % of the participants reported sleeping for at least eight hours once or twice a week, while 82,68 % did not engage in physical exercise. Resident physician constituted 45,67 % of the sample, and the median professional experience in Primary Care was 8 years (IQR: 3-17). A noteworthy proportion (87,40 %) of the workers expressed dissatisfaction with their economic income. Further details regarding sociodemographic characteristics, lifestyle, and professional features are presented in table 1.
|
Table 1. Sample distribution according to sociodemographic characteristics, lifestyle, and professional features |
|||
|
Variable |
No. (%) |
||
|
Sociodemographic characteristics |
Age |
|
31 (27-41)* |
|
Sex |
Female |
85 (66,93) |
|
|
Male |
42 (33,07) |
||
|
Skin color |
White |
101 (79,53) |
|
|
Mixed race |
13 (10,24) |
||
|
Black |
13 (10,24) |
||
|
Religion |
Atheist |
62 (48,82) |
|
|
Catholic |
10 (7,87) |
||
|
Christian |
36 (28,35) |
||
|
Other |
19 (14,96) |
||
|
Marital status |
Married/Common-law |
72(56,69) |
|
|
Divorced |
5 (3,94) |
||
|
Single |
50 (39,37) |
||
|
Lifestyle |
Parental status |
Yes |
47 (37,01) |
|
|
No |
80 (62,99) |
|
|
|
Sleeping eight hours daily |
> 4 times a week |
23 (18,11) |
|
|
3-4 times a week |
30 (23,62) |
|
|
|
1-2 times a week |
43 (33,86) |
|
|
|
Never |
31 (24,41) |
|
|
|
Practice of physical exercise |
Yes |
22 (17,32) |
|
|
No |
105 (82,68) |
|
|
|
Presence of smoking |
Yes |
18 (14,17) |
|
|
No |
109 (85,83) |
|
|
|
Adequate dietary habits |
Yes |
11 (8,66) |
|
|
No |
116 (91,34) |
|
|
Professional characteristics |
Profession |
Specialist physician |
46 (36,22) |
|
Resident physician |
58 (45,67) |
||
|
Nurse |
14 (11,02) |
||
|
Other |
9 (7,09) |
||
|
Satisfaction with economic income |
Yes |
7 (5,51) |
|
|
Partially |
9 (7,09) |
||
|
No |
111 (87,40) |
||
|
|
Professional experience |
|
8 (3-17)* |
|
Notes: * Median (Interquartile range) |
|||
In the examined sample (figure 1), a prevailing presence of individuals experiencing BS was observed, accounting for (73,23 %). Figure 2 depicts the distribution of the sample based on the impact on various assessed dimensions, with Emotional Exhaustion (EE) being the most affected (92,13 %).
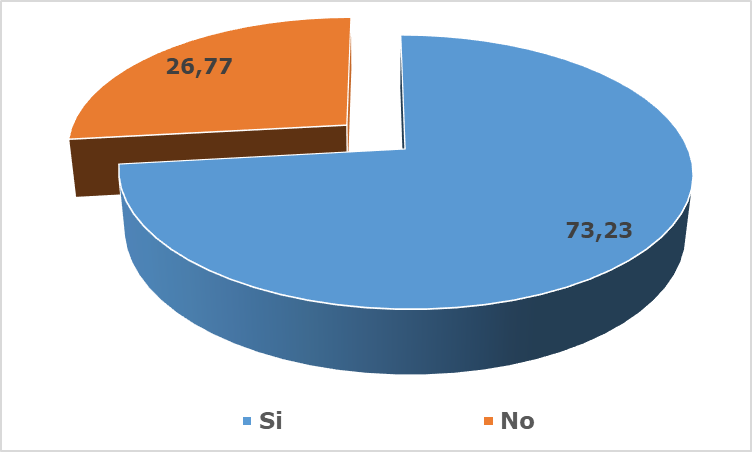
Figure 1. Sample distribution based on the presence of Burnout Syndrome
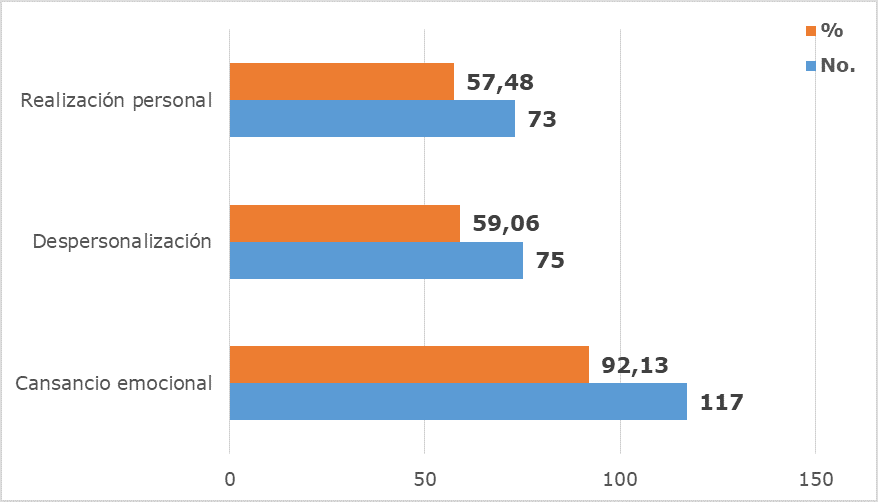
Figure 2. Sample distribution according to the presence of affectation in each dimension of the Maslach Burnout Inventory questionnaire
The prevalence of burnout was higher among women (77,65 %), individuals with black skin color (100 %), Christians (77,78 %), and singles (80,0 %). Similarly, higher percentages of burnout were observed among individuals with children (78,72 %), those who took care of others (77,55 %), and those who never slept at least eight hours daily (90,32 %). Medical residents (79,31 %) and individuals partially satisfied with their income (77,78 %) also exhibited a higher percentage of burnout. Table 2 illustrates the remaining relationships between lifestyle, sociodemographic, and professional characteristics with the presence of burnout. The only variables that displayed a statistically significant association with the presence of burnout were not sleeping eight hours daily (p=0,016) and being dissatisfied with economic income (p<0,001).
|
Table 2. Presence of BS according to lifestyle, sociodemographic variables, and professional characteristics |
||||
|
Variable |
Presence of Burnout Syndrome |
p |
||
|
Yes |
No |
|||
|
No. (%) |
No. (%) |
|||
|
Age |
31 (27-40) |
34 (27,75-42,25) |
0,277€ |
|
|
Sex |
Female |
66 (77,65) |
19 (22,35) |
0,110β |
|
Male |
27 (64,29) |
15 (35,71) |
||
|
|
|
|
|
|
|
Skin color |
White |
71 (70,30) |
30 (29,70) |
0,071β |
|
Mixed race |
9 (69,23) |
4 (30,77) |
||
|
Black |
13 (100) |
0 (0) |
||
|
Religion |
Atheist |
48 (77,42) |
14 (22,58) |
0,165β |
|
Catholic |
7 (70,0) |
3 (30,0) |
||
|
Christian |
28 (77,78) |
8 (22,22) |
||
|
Other |
10 (52,63) |
9 (47,37) |
||
|
Marital status |
Married/Common-law |
51 (70,83) |
21 (29,17) |
0,123β |
|
Divorced |
2 (40,0) |
3 (60,0) |
||
|
Single |
40 (80,0) |
10 (20,0) |
||
|
Parental status |
Yes |
37 (78,72) |
10 (21,28) |
0,284β |
|
No |
56 (70,0) |
24 (30,0) |
||
|
Sleeping eight hours daily |
> 4 times a week |
12 (52,17) |
11 (47,83) |
0,016β |
|
3-4 times a week |
23 (76,67) |
7 (23,33) |
||
|
1-2 times a week |
30 (69,77) |
13 (30,23) |
||
|
Never |
28 (90,32) |
3 (9,68) |
||
|
Practice of physical exercise |
Yes |
15 (68,18) |
7 (31,82) |
0,557β |
|
No |
78 (74,29) |
27 (25,71) |
||
|
Presence of smoking |
Yes |
17 (94,44) |
1 (5,56) |
0,057£ |
|
No |
76 (69,72) |
33 (30,28) |
||
|
Adequate dietary habits |
Yes |
8 (72,73) |
3 (27,27) |
0,969β |
|
No |
85 (73,28) |
31 (26,72) |
||
|
Profession |
Specialist physician |
33 (71,74) |
13 (28,26) |
0,363β |
|
Resident physician |
46 (79,31) |
12 (20,69) |
||
|
Nurse |
8 (57,14) |
6 (42,86) |
||
|
Other |
6 (66,67) |
3 (33,33) |
||
|
Professional experience |
8 (3-17) |
9,50 (3,75-18,25) |
0,300€ |
|
|
Satisfaction with economic income |
Yes |
0 (0) |
7 (100) |
< 0,001β |
|
Partially |
7 (77,78) |
2 (22,22) |
||
|
No |
86 (77,48) |
25 (22,52) |
||
|
Notes: βPearson’s Chi-square; €U Mann Whitney; £Yates’ correction |
||||
Table 3 presents the distribution of study participants exhibiting impairment in various domains of the questionnaire based on their lifestyle, sociodemographic, and professional variables. The impact of the EE domain was associated with sex (p=0,038), religion (p=0,002), and daily sleep duration of eight hours (p<0,001). The Depersonalization (DP) dimension showed association with religion (p=0,001), daily sleep duration of eight hours (p=0,016), smoking (p=0,001), and satisfaction with economic income (p=0,011). Meanwhile, the Reduced Personal Accomplishment (PA) dimension was linked to daily sleep duration of eight hours (p<0,001), adequate dietary habits (p=0,038), and satisfaction with economic income (p=0,016).
|
Table 3. Affected domains of Maslach Burnout Inventory questionnaire according to lifestyle, sociodemographic variables, and professional characteristics |
|||||||
|
Variable |
Domains |
||||||
|
Emotional exhaustion (n=117) |
Depersonalization (n=75) |
Personal Accomplishment (n=73) |
|||||
|
No. (%) |
p |
No. (%) |
p |
No. (%) |
p |
||
|
Sexβ |
Female |
80 (94,12) |
0,038 |
50 (58,82) |
0,252 |
52 (61,18) |
0,247 |
|
Male |
37 (88,10) |
25 (59,52) |
21 (50,0) |
||||
|
Age€ |
31 (27-40)* |
0,435 |
31 (27-41)* |
0,389 |
31 (27-39,50)* |
0,055 |
|
|
Skin Color£ |
White |
93 (92,08) |
0,123 |
57 (56,44) |
0,553 |
57 (56,44) |
0,482 |
|
Mixed-race |
11 (84,62) |
7 (53,85) |
6 (46,15) |
||||
|
Black |
13 (100) |
11 (84,62) |
10 (76,92) |
||||
|
Religion£ |
Atheist |
55 (88,71) |
0,002 |
48 (77,42) |
0,001 |
29 (46,77) |
0,318 |
|
Catholic |
10 (100) |
4 (40,0) |
7 (70,0) |
||||
|
Christian |
33 (91,67) |
18 (50,0) |
28 (77,78) |
||||
|
Other |
19 (100) |
5 (26,32) |
9 (47,37) |
||||
|
Marital Status£ |
Married/Common- law |
65 (90,28) |
0,389 |
43 (59,72) |
0,368 |
36 (50,0) |
0,089 |
|
Divorced |
2 (40,0) |
2 (40,0) |
2 (40,0) |
||||
|
Single |
50 (100) |
30 (60,0) |
35 (70,0) |
||||
|
Parental statusβ |
Yes |
42 (89,36) |
0,233 |
29 (61,70) |
0,774 |
32 (68,09) |
0,337 |
|
No |
75 (93,75) |
46 (57,50) |
41 (51,25) |
||||
|
Sleeping Eight Hours Daily£ |
> 4 times a week |
20 (86,96) |
<0,001 |
10 (43,48) |
0,016 |
4 (17,39) |
<0,001 |
|
3-4 times a week |
26 (86,67) |
18 (60,0) |
20 (66,67) |
||||
|
1-2 times a week |
43 (100) |
24 (55,81) |
21 (48,84) |
||||
|
Never |
28 (90,32) |
23 (74,19) |
|
28 (90,32) |
|
||
|
Practice of physical exercise β |
Yes |
17 (77,27) |
0,267 |
15 (68,18) |
0,452 |
11 (50,0) |
0,421 |
|
No |
100 (95,24) |
60 (57,14) |
62 (59,05) |
||||
|
Presence of smoking β |
Yes |
18 (100) |
0,303 |
17 (94,44) |
0,001 |
11 (61,11) |
0,152 |
|
No |
99 (90,83) |
58 (53,21) |
62 (56,88) |
||||
|
Adequate dietary habits β |
Yes |
11 (100) |
0,068 |
8 (72,73) |
0,430 |
3 (27,27) |
0,038 |
|
No |
106 (91,38) |
67 (57,76) |
70 (60,34) |
||||
|
Profession£ |
Specialist physician |
42 (91,30) |
0,491 |
26 (56,52) |
0,336 |
25 (54,35) |
0,382 |
|
Resident physician |
56 (96,55) |
38 (65,52) |
36 (62,07) |
||||
|
Nurse |
11 (78,57) |
5 (35,71) |
6 (42,86) |
||||
|
Other |
8 (88,89) |
6 (66,67) |
6 (66,67) |
||||
|
Professional experience € |
8 (3-17)* |
0,796 |
7 (3-17)* |
0,412 |
8 (3-16,50)* |
0,120 |
|
|
Satisfaction with economic income£ |
Yes |
5 (71,43) |
0,506 |
0 (0) |
0,011 |
0 (0) |
0,016 |
|
Partially |
7 (77,78) |
7 (77,78) |
7 (77,78) |
||||
|
No |
105 (94,59) |
68 (61,26) |
66 (59,46) |
||||
|
Notes: βMann-Whitney U, €Spearman’s Correlation, £ Kruskal Wallis H |
|||||||
DISCUSSION
Personnel in primary care health services contend with a range of intricate tasks in their daily responsibilities, influenced by various stressors that necessitate high emotional involvement. Additionally, their interactions with patients expose them to an excess of aversive stimulation.(19) Notably, the observed prevalence of BS in the obtained results surpasses that reported in national studies,(16,17) regional studies,(20,21) and global studies.(10,12,22) This condition poses a twofold increase in the risk of adverse incidents for patient safety and results in an overall decline in the quality of care, coupled with a decrease in patient satisfaction.(23)
The current study reports higher percentages of affectation in the evaluated domains compared to data reported in the literature.(24,25,26) Abdulrahman et al.(27) documented similar results in the United Arab Emirates, where 70 % of participants reported experiencing BS, 75,5 % reported emotional exhaustion, 84 % reported high depersonalization, and 74 % reported a diminished sense of personal accomplishment.
In terms of demographic characteristics, the prevalence of women,(1,5) individuals over 40 years old,(28) those with a partner,(10) having children,(3,29) and having dependents,(6) aligns with what is described in the literature. Regarding lifestyle, Ovejas-López et al.(5) found that 26,8 % of workers in their sample maintain low physical activity, only 3,3 % sleep at least eight hours per day, and 12,2 % are smokers.
Concerning sex, this research revealed a higher prevalence of BS in females compared to males (77,65 % versus 64,29 %). This trend aligns with the findings of Ramírez Pérez et al.(6) who demonstrated that the overall risk of Burnout is 3,692 times higher in women than in men (95% CI: 1,30–10,49), and these sex differences are statistically significant (p=0,011). Regarding the analysis of the comparison of means for the dimensions comprising the Maslach Burnout Inventory (MBI), Llor Lozano et al.(19) specify that in men, depersonalization and personal accomplishment exhibit lower results compared to females, which coincides with findings in healthcare workers belonging to Primary Care Teams in the Central Catalonia Health Region.(2)
In relation to age, Cañadas de la Fuente et al.(4) reported significant differences (p=0,015) between age and the EE dimension, wherein all conducted comparisons indicated that the younger age group exhibited a lower level of EE. A similar result is reported by Nwosu et al.(30) who found in their study that respondents in the age group of 35–39 years had the highest mean disengagement score, 2,5±0,4, and the difference in the mean was statistically significant (F = 3,183; p = 0,042).
Regarding self-care practices or lifestyles, Chung et al.(31) emphasize the significance of factors such as sleep duration, the frequency of physical activity or exercise, a proper diet, and the abandonment of certain toxic habits like smoking. Although the latter two have not showed strong support in the literature, the quantity and quality of sleep, along with regular engagement in physical exercise, are considered crucial elements in the genesis of BS, even though individuals often tend to underestimate their impact.
Physician burnout has been attributed to various factors including excessive workloads, unpredictable schedules, conflicts between work and home, among others. More recently, the impact of sleep and circadian disorders has come to light, revealing an increased risk of burnout and, consequently, medical errors, among those workers with sleep disorders. Recognizing this, the American Academy of Sleep Medicine (AASM) has called for more research into the roles of sleep disruption, sleep deprivation, and circadian misalignment in physician burnout. In this context, Shi et al.(32) in bivariate analysis, demonstrate a correlation between sleep duration and the EE dimension (p=0,018), although the remaining dimensions did not exhibit the same behavior [DP (p=0,152) and PA (p=0,643)].
While few adults achieve the recommended 8 hours of sleep per night, doctors, on average, only manage 6,5 hours per night. According to a national survey conducted by the American College of Chest Physicians Sleep Institute, one in five doctors reported missing family or leisure activities due to sleep problems. This situation can be particularly challenging for doctors who naturally have an advanced sleep phase (the "morning person") or a delayed sleep phase (the "night owl") of the circadian rhythm. The health effects associated with sleep deprivation are similar to the findings of burnout and include mood changes, increased drowsiness, fatigue, irritability, difficulty concentrating, and disorientation.(33,34)
Regarding work characteristics, a systematic review conducted in Ibero-America between 2012 and 2018, encompassing 23 evaluated studies with 3516 workers, revealed that 46 % were medical specialists.(35) In terms of professional category, a multicenter study in Health Areas of Castilla-La Mancha demonstrated a higher prevalence of burnout among physicians compared to the nursing collective. The authors of that study suggested that this difference could be associated with the distinct functions or responsibilities carried out by physicians. However, when considering the rest of the possible confounding or interacting factors, this relationship may not persist.(24) Conversely, other studies outline how adherence to medical indications makes nursing staff more prone to developing BS.(19,36) It is within this professional category that the highest percentages of EE are observed according to Cañadas de la Fuente et al.(4)
The presence of BS is not synonymous with the existence of psychological stress but rather a response to chronic occupational stressors stemming from professional-patient relationships. As this exposure extends, the rate of burnout tends to escalate.(37) In this context, Garcia-Molina et al.(21) compared the burnout percentage in each subscale with the labor-related variables of interest. The results unveiled a higher prevalence of Depersonalization in individuals who had been working between 10 and 20 years (55,6 %, p=0,033).
In a multicenter study conducted in Nigeria, it was identified that engaging in professional practice for more than 10 years is correlated with the manifestation of EE.(30) Likewise, Muraya Alshreem and colleagues(28) indicate in their study that participants who had been practicing for more than ten years exhibited heightened levels of emotional exhaustion (30,7 %; p=0,008), coupled with a high rate of reduced personal accomplishment (67,7 %; p=0,046).
Álvarez Mena et al.(35) state that in 17,3 % of the studies included in their systematic review, a good or bad salary was considered a variable significantly correlated with the onset of BS (p<0,05). This observation resonates with the findings in the present study, where among the labor characteristics, salary emerges as one of the factors with the most substantial impact on the occurrence of this phenomenon. This finding has been documented by other sources.(22,38)
These findings align with previous research, which found that burnout is primarily influenced by the work environment rather than personal factors, confirming that burnout is more of a social problem than an individual one.(28,39)
Among the limitations outlined in this present study was the inability to integrate additional health sectors within the municipality (and undertake a multicenter study), which could have yielded a more comprehensive understanding of the phenomenon in the investigated region. The nature of the conducted study, being cross-sectional, constrained the evaluation of temporality and causality relationships. Another limitation of the study was the incapacity to incorporate other predictive variables (such as job pressure, self-esteem, stress, and anxiety, among others). Finally, there exists the possibility of social desirability bias due to the stigma associated with reporting on occupational burnout among healthcare personnel.
CONCLUSIONS
The current study identified the lifestyle, demographic, and professional attributes of healthcare personnel. The presence of burnout syndrome was evaluated, and it was found to be predominant among the study participants, with its occurrence notably associated with not sleeping eight hours daily and dissatisfaction with economic income. Notably, emotional exhaustion emerged as the dimension most profoundly affected within the Maslach Burnout Inventory questionnaire. The analyzed individuals’ characteristics were related to each dimension, affirming the existence of associations between them. The obtained results contribute to a better understanding of the dynamics of this phenomenon within Primary Care service providers, facilitating more effective management. This, in turn, ensures enhanced service delivery and contributes to an overall improvement in their quality of life.
REFERENCES
1. Ortega-Campos E, Cañadas-De la Fuente G, Albendín-García L, Gómez-Urquiza J, Monsalve-Reyes C, Inmaculada de la Fuente-Solana E. A Multicentre Study of Psychological Variables and the Prevalence of Burnout among Primary Health Care Nurses. Int. J. Environ. Res. Public Health. 2019; 16: e3242. DOI: 10.3390/ijerph16183242
2. Roig-Grau I, Fornés-Ollé B, Rodriguez-Roig R, Delgado-Juncadella A, González-Valero J, Rodríguez-Martín I. Burnout en profesionales de atención primaria en la Cataluña Central. Arch Prev Riesgos Labor. 2022; 25(2): 86-100. DOI: 10.12961/aprl.2022.25. 02.02
3. Abarca Mato R, Emigdio Vargas A, Dávalos Martínez A, Barrera Rodríguez E, Morales López F, Blanco García N. Síndrome de burnout en profesionales sanitarios en formación de un hospital público en Acapulco, México. Rev. Cuba. Salud Trab. 2023; 24(1). Disponible en: https://revsaludtrabajo.sld.cu/index.php/revsyt/article/view/363
4. Cañadas-de la Fuente G, San Luis C, Lozano L, Vargas C, García I, de la Fuente EI. Evidencia de validez factorial deMaslach Burnout Inventory y estudio de los niveles de burnout en profesionales sanitarios. Rev Latinoam Psicol. 2014; 46(1): 44-52. DOI: 10.1016/S0120-0534(14)70005-6
5. Ovejas-López A, Izquierdo F, Rodríguez-Barragán M, Rodríguez-Benítez J, García-Batanero M, Alonso-Martínez A, et al. Burnout y malestar psicológico en los residentes de Medicina Familiar y Comunitaria. Aten Primaria. 2020; 52(9): 608-616. DOI: 10.1016/j.aprim.2020.02.014
6. Ramírez Pérez M, Garicano Quiñónez L, González de Abreu J, Jiménez González de Buitrago E, Sánchez Úriz M, del Campo Balsa M. Síndrome de burnout en médicos residentes de los hospitales del área sureste de la Comunidad de Madrid. Rev Asoc Esp Espec Med Trab. 2019; 28: 57-65. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S1132-62552019000100007&lng=es
7. Jácome S, Villaquiran-Hurtado A, García C, Duque I. Prevalencia del síndrome de Burnout en residentes de especialidades médicas. Rev Cuid. 2019; 10(1): e543. Disponible en: http://www.scielo.org.co/scielo.php?pid=S2216-09732019000100200&script=sci_arttext
8. Rodrigues H, Cobucci R, Oliveira A, Cabral J, Medeiros L, Gurgel K, et al. Burnout syndrome among medical residents: a systematic review and metaanalysis. PLoS One. 2018; 13(11): e0206840. DOI: 10.1371/journal.pone.0206840
9. Molina-Praena J, Ramirez-Baena L, Gomez-Urquiza J, Canadas G, De la Fuente E, Canadas-De la Fuente G. Levels of Burnout and Risk Factors in Medical Area Nurses: A Meta-Analytic Study. Int J Environ Res Public Health. 2018; 15(12). DOI: 10.3390/ijerph15122800
10. AL-Haddad A, AL-Omar F, AL-Khaleel A, AL-Khalaf A. Prevalence of burnout syndrome and its related risk factors among physicians working in primary health care centers of the Ministry of Health, Al Ahsa region, Saudi Arabia, 2018–2019. J Family Med Prim Care. 2020; 9: 517-519. DOI: 10.4103/jfmpc.jfmpc_743_19
11. Sullivan E, McKinstry D, Adamson J, Hunt L, Phillips R, Linzer M. Burnout Among Missouri Primary Care Clinicians in 2021: Roadmap for Recovery? Medicine. 2022; 119(4): 397-400. Disponible en: https://pubmed.ncbi.nlm.nih.gov/36118800/
12. Grumbach K, Knox M, Huang B, Hammer H, Kivlahan C, Willard-Grace R. A Longitudinal Study of Trends in Burnout During Primary Care Transformation. Ann Fam Med. 2019; 17: S9-S16. DOI: 10.1370/afm.2406
13. Woodward R, Cheng T, Fromewick J, SL G, Latessa R. What happy physicians have in common: A qualitative study of workplace perceptions of physicians with low burnout scores. SAGE Open Medicine. 2022; 10: 1-9. DOI: 10.1177/20503121221085841
14. Chemali Z, Ezzeddine F, Gelaye B, Dossett M, Salameh J, Bizri M. Burnout among healthcare providers in the complex environment of the Middle East: a systematic review. BMC Public Health. 2019; 19: e1337. DOI: 10.1186/s12889-019-7713-1
15. Juárez-García A, Merino-Soto C, Fernández-Arata M, Flores-Jiménez C, Caraballo M, Camacho-Cristiá C. Validación transcultural y funcionamiento diferencial del Maslach Burnout Inventory - General Survey en docentes de tres países latinoamericanos. Av. Psicol. Latinoam. 2020; 38(1): 135-158. Disponible en: http://www.scielo.org.co/scielo.php?pid=S1794-47242020000100135&script=sci_arttext
16. JR H. Estrés y Burnout en profesionales de la salud de los niveles primario y secundario de atención. Rev Cubana Salud Pública. 2003; 29(2): 103-110. Disponible en: http://scielo.sld.cu/scielo.php?pid=S0864-34662003000200002&script=sci_arttext&tlng=en
17. Pando Moreno M, Aranda Beltrán C, López Palomar M. Validez factorial del Maslach Burnout Inventory-General Survey en ocho países Latinoamericanos. Cienc Trab. 2015; 17(52): 28-31. Disponible en: https://www.scielo.cl/scielo.php?pid=S0718-24492015000100006&script=sci_arttext&tlng=pt
18. Peacok Aldana A, Cala Calviño L, Labadié Fernández S, Álvarez Escalante L. Ética en la investigación biomédica: contextualización y necesidad. MEDISAN. 2019; 23(5): 921-941. Disponible en: http://scielo.sld.cu/scielo.php?pid=S1029-30192019000500921&script=sci_arttext
19. Llor Lozano J, Seva Llor A, Díaz Agea J, Llor Gutiérrez L, Leal Costa C. Burnout, habilidades de comunicación y autoeficacia en los profesionales de urgencias y cuidados críticos. Enfermería Global. 2020 Jul;(59): 68-80. Disponible en: https://scielo.isciii.es/scielo.php?pid=S1695-61412020000300068&script=sci_arttext
20. Loya-Murguía K, Valdez-Ramírez J, Bacardí- Gascón M, Jiménez-Cruz A. El síndrome de agotamiento en el sector salud de Latinoamérica: revisión sistemática. JONNPR. 2018; 31(1): 40-48. Disponible en: https://revistas.proeditio.com/jonnpr/article/view/2060
21. Berrío García N, Foronda Valencia D, Ciro Parra D. Síndrome de burnout en personal de la salud latinoamericano. Revista de Psicología. 2018; 10(2): 157-181. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=7529914
22. Yates S. Physician Stress and Burnout. Am J Med. 2020; 133(2): 160-164.
23. Willard-Grace R, Knox M, Huang B, Hammer H, Kivlahan C, Grumbach K. Burnout and Health Care Workforce Turnover. Ann Fam Med. 2019; 17(1): 36-41. DOI: 10.1370/afm.2338
24. Párraga-Martínez I, González-Hidalgo E, Méndez-García T, Villarín-Castro A, LeónMartín A. Burnout y su relación con el estrés percibido y la satisfacción laboral en profesionales sanitarios de Atención Primaria de una Comunidad Autónoma. Rev Clín Med Fam. 2018; 11(2): 51-60. Disponible en: https://scielo.isciii.es/scielo.php?pid=S1699-695X2018000200051&script=sci_arttext&tlng=pt
25. Soltanifar A, Pishbin E, Attaran Mashhadi N, Najaf Najafi M, Siahtir M. Burnout among female emergency medicine physicians: a nationwide study. Emerg Med Australas. 2018; 30(4): 517-522. DOI: 10.1111/1742-6723.12941
26. García-Molina C, Satorres-Pérez M, Crespo-Mateos A, Quesada Rico J, García-Soriano L, Carrascosa-Gonzalvo S. Prevalencia del síndrome de burnout en profesionales de medicina y enfermería de Atención Primaria en centros de salud acreditados para Formación Sanitaria Especializada de dos áreas de salud de Alicante. Rev Clin Med Fam. 2022; 15(1): 35-39. Disponible en: https://scielo.isciii.es/scielo.php?pid=S1699-695X2022000100007&script=sci_arttext&tlng=en
27. Abdulrahman M, Nair S, Farooq M, Al Kharmiri A, Al Marzooqi F, Carrick F. Burnout and depression among medical residents in the United Arab Emirates: a multicenter study. J Family Med Prim Care. 2018; 7(2): 435-441. DOI: 10.4103/jfmpc.jfmpc_199_17
28. Muraya Alshreem R, Baraja M, Solaiman Almogbel E. Prevalence of burnout and its impact on self-reported patient care among primary health care physicians at King Abdul-Aziz Medical City in Riyadh region. J Family Med Prim Care. 2022; 11(8): 4624–4630. DOI: 10.4103/jfmpc.jfmpc_1622_21
29. Pintarić Japec V, Vučemilo L, Kust D, Babacanli A, Dodig D, Štefančić V, et al. Burnout among Croatian physicians: a cross-sectional national survey. Croat Med J. 2019; 60(3): 255-264. DOI: 10.3325/cmj.2019.60.255
30. Nwosu A, Ossai E, Mba U, Anikwe I, Ewah R, Obande B, et al. Physician burnout in Nigeria: a multicentre, cross-sectional study. BMC Health Serv Res. 2020;(20): 863. DOI: 10.1186/s12913-020-05710-8
31. Chung S, Dillon E, Meehan A, Nordgren R, Frosch D. The Relationship Between Primary Care Physician Burnout and Patient-Reported Care Experiences: a Cross-sectional Study. J Gen Intern Med. 2020; 35(8): 2357-2364. DOI: 10.1007/s11606-020-05770-w
32. Shi C, Luo J, Xiao Y. The association of sleep quality and burnout among Chinese medical residents under standardized residency training in a tertiary hospital. Sleep Breath. 2023; 27(1): 379-386. DOI: 10.1007/s11325-022-02621-2
33. Stewart N, Arora V. The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest. 2019; 156(5): 1022-1030. DOI: 10.1016/j.chest.2019.07.008
34. Trockel M, Menon N, Rowe S, Stewart M, Smith R, Lu M, et al. Assessment of Physician Sleep and Wellness, Burnout, and Clinically Significant Medical Errors. JAMA Netw Open. 2020; 3(12): e2028111. DOI: 10.1001/jamanetworkopen.2020.28111
35. Álvarez Mena J, Cobo Molina N, Parra Osorio L, Gómez Salazar L, Acosta Fernández M. Prevalencia del síndrome de Burnout en médicos iberoamericanos entre 2012 y 2018: una revisión sistemática. Revista Diálogos de Saberes. 2019;(50): 39-60. Disponible en: https://revistas.unilibre.edu.co/index.php/dialogos/article/view/5551
36. Intriago Miranda S. Síndrome del “Burnout” en personal de salud de un centro hospitalario de la dirección distrital Junín-Bolívar. Revista San Gregorio. 2019; 35: 94-107. Disponible en: http://scielo.senescyt.gob.ec/scielo.php?pid=S2528-79072019000200094&script=sci_arttext
37. Martínez Melero M. Síndrome de Burnout en profesiones sanitarias. Enfermería y medicina como población diana. Rev. sanit. investig. 2021; 12(2): e181. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=8277533
38. Nicholls M. Cardiologists and the Burnout scenario. Eur Heart J. 2019; 40(1): 5-6. DOI: 10.1093/eurheartj/ehy788
39. Polacov S, Barrionuevo Battistini I, Barroso G, Cravero B, D’Alessandro T, Allende G, et al. Riesgo de Síndrome de Burnout en profesionales médicos de la ciudad de Córdoba, Argentina. Rev Fac Cien Med Univ Nac Cordoba. 2021; 78(4): 371-375. DOI: 10.31053/1853.0605.v78.n4.28749
Funding
No financing.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
AUTHORSHIP CONTRIBUTION
Conceptualization: Lázaro Pablo Linares Cánovas, Liyansis Bárbara Linares Cánovas, Yoelys Pereda Rodríguez, Beatriz Gallardo Hernández, Martha María Pérez Martín, Adalina Linares Montano.
Research: Lázaro Pablo Linares Cánovas, Liyansis Bárbara Linares Cánovas, Yoelys Pereda Rodríguez, Beatriz Gallardo Hernández, Martha María Pérez Martín, Adalina Linares Montano.
Methodology: Lázaro Pablo Linares Cánovas, Liyansis Bárbara Linares Cánovas, Yoelys Pereda Rodríguez, Beatriz Gallardo Hernández, Martha María Pérez Martín, Adalina Linares Montano.
Original drafting and editing: Lázaro Pablo Linares Cánovas, Liyansis Bárbara Linares Cánovas, Yoelys Pereda Rodríguez, Beatriz Gallardo Hernández, Martha María Pérez Martín, Adalina Linares Montano.
Writing, editing and proofreading: Lázaro Pablo Linares Cánovas, Liyansis Bárbara Linares Cánovas, Yoelys Pereda Rodríguez, Beatriz Gallardo Hernández, Martha María Pérez Martín, Adalina Linares Montano.